Maintaining Your Medicaid Coverage
If you fail to report life changes you could lose your Medicaid coverage, even if those changes don’t actually impact your eligibility.
Medicaid Buy In Program For Working People With Disabilities And Medicare Savings Programs
The Medicaid Buy-In Program for Working People with Disabilities provides Medicaid coverage for people ages 16-64 who have a disability and are engaged in a work activity for which they are paid. In order to be considered for this program, the individual must be determined disabled as defined by the Social Security Administration. The persons net income must be at or below 250% of the federal poverty level.
How Do I Apply For Medicaid
You can apply for Medicaid in any one of the following ways:
- Write, phone, or go to your local department of social services.
- In New York City, contact the Human Resources Administration by calling 557-1399.
- Pregnant individuals and children can apply at many clinics, hospitals, and provider offices. Call your local department of social services to find out where you can apply.
> >
Don’t Miss: How To Break A Lease In New York State
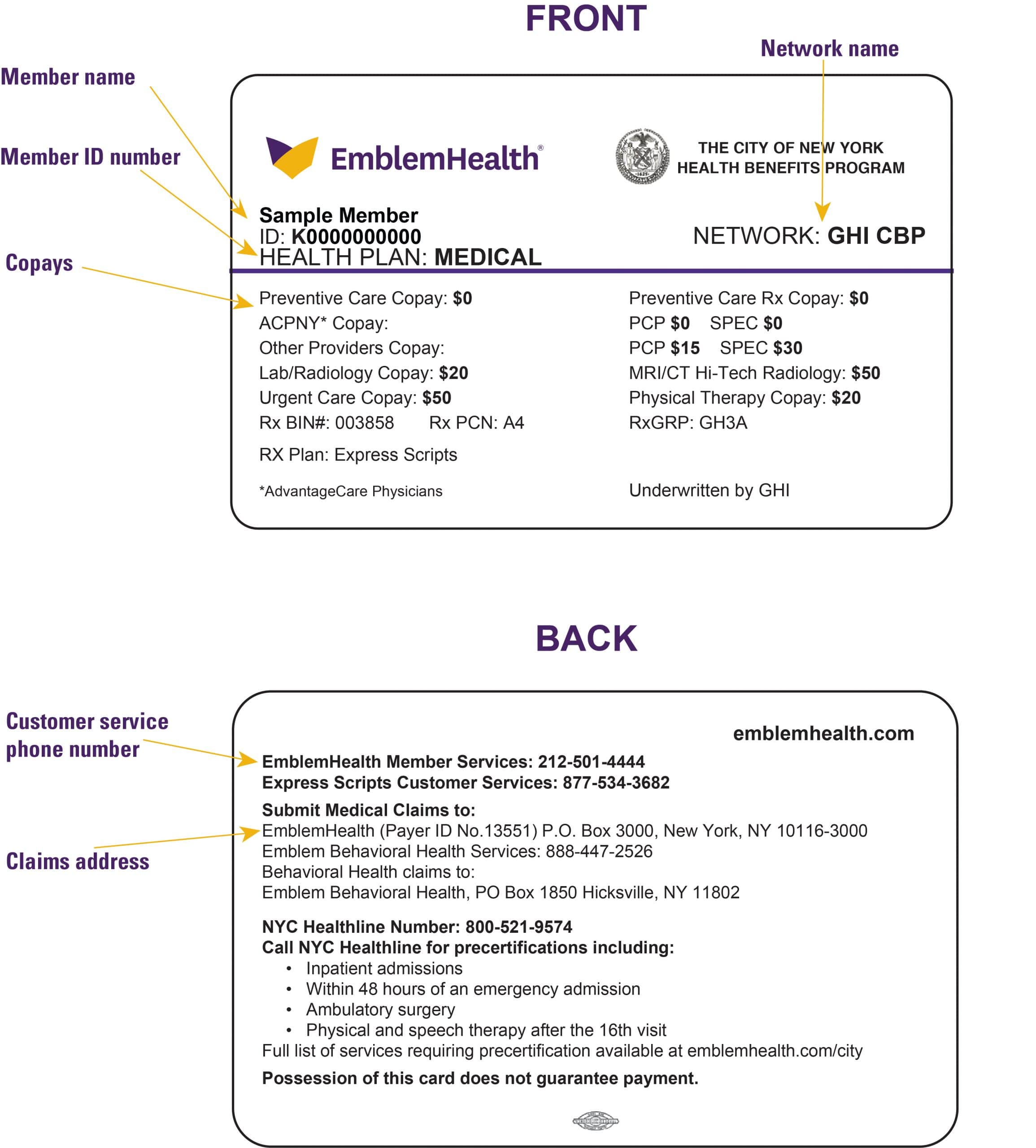
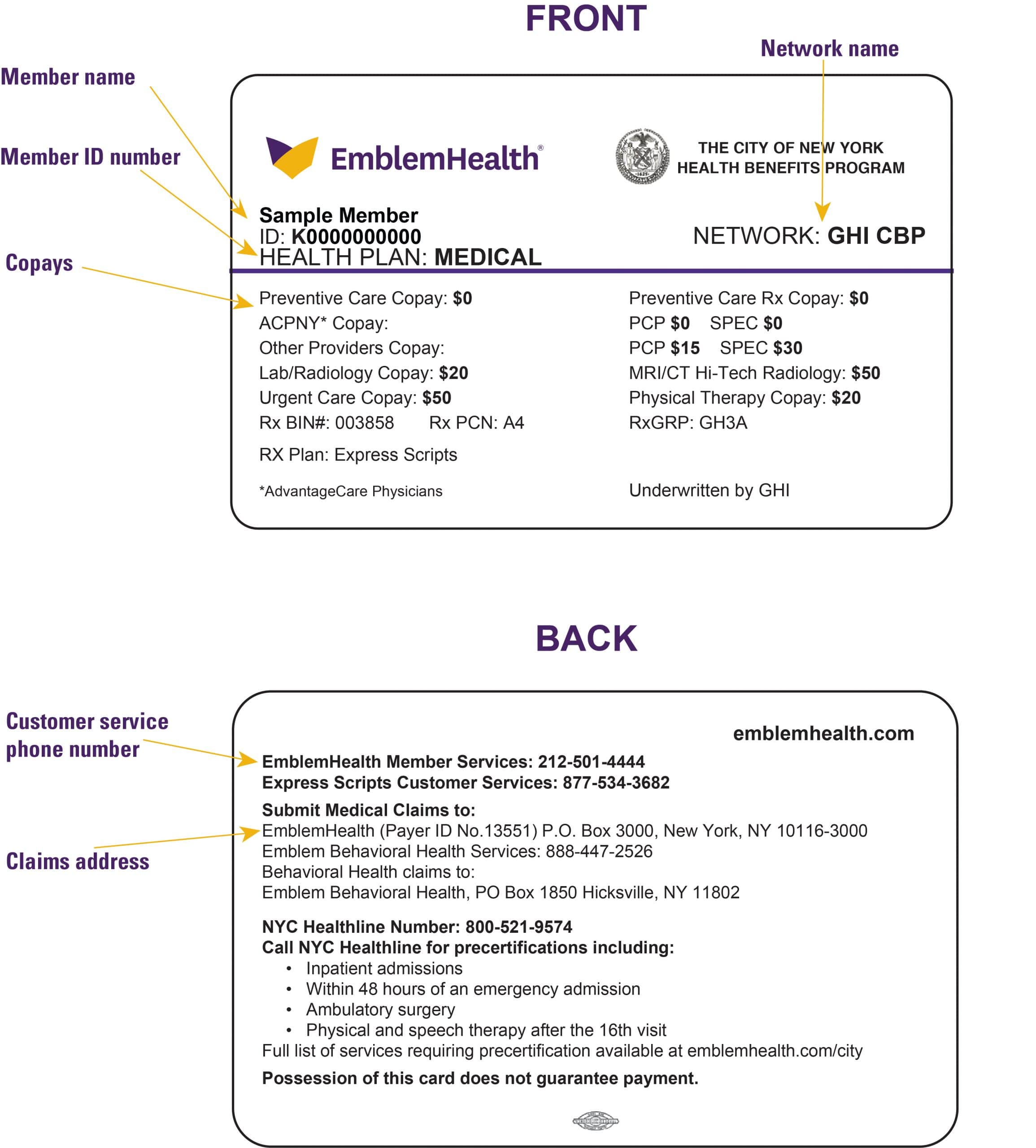
Best Medicaid Health Plan Ny
Most people with NYS Medicaid will have the chance to select a Managed Care plan. The biggest difference between each plan available in your county will be the network. Not every doctor will accept every plan. If you already have a doctor that you like, be sure to find out which NYS Medicaid Managed Care plans your doctor accepts. The basic benefits will be the same for most of these plans, but the best plan may not be the same for you as it is for your neighbor. For example, some plans include family planning services, but others may not.
When you select a Managed Care Plan, youll have to select one primary physician who will be the main doctor that you will go to first for most of your health care needs. That doctor can give you referrals for specialists.
You should receive a package about the plans you can choose from when you are accepted into the New York Medicaid program.
Overview Medicaid For Seniors In Ny
While Medicaid programs target different groups of people, this report is concerned only with long-term care that benefits the seniors and elderly, with a focus on the state of New York. Medicaid is a joint venture between the Federal government and each state, catering mostly to low-income people. The Federal government provides subsidies and sets basic standards while, generally speaking, each state sets eligibility requirements and other rules that govern services. Some 66 million people received Medicaid benefits in 2018, of those 7.2 million , making it the largest payer of healthcare benefits in the United States.
Here is a brief summary of the type of elderly-related programs that Medicaid offers in the state of New York:
- Nursing homes: If you are a senior or elderly Medicaid beneficiary, Medicaid has traditionally paid for long-term care in all Medicaid-certified nursing homes or senior living homes.
- Home-based programs:For at-home care, Medicaid has several programs in the state of New York for seniors and elderly that cover home health care as well as personal care .
Home and community-based programs: In 2018, every state in the country, as well as D.C., offered at least one program that pays for elderly-related services for those who choose not to become nursing home residents. The state of New York has various programs that provide assistance at home for seniors, in assisted living facilities , in day care, and with other home-related chores.
Also Check: How To Order A Death Certificate In New York
Applying For Ny Medicaid Long Term Care Programs
The first step in applying for a NY Medicaid Long Term Care program is deciding which of the three programs discussed above you or your loved one want to apply for Nursing Home Medicaid, Home and Community Based Service Waivers or Disabled, Aged 65+ or Blind / Regular Medicaid.
The second step is determining if the applicant meets the financial and functional criteria, also discussed above, for that Long Term Care program. Applying for NY Medicaid when not financially eligible will result in the application, and benefits, being denied.
During the process of determining financial eligibility, its important to start gathering documentation that clearly details the financial situation for the NY Medicaid applicant. These documents will be needed for the official NY Medicaid application. Necessary documents include five years of quarterly bank statements from all accounts the most recent monthly or quarterly statements from all investments, IRAs, 401Ks, annuities and any other financial accounts a letter from the Social Security Administration showing the applicants gross Social security income and deductions tax forms to verify income streams including wages, pensions, royalties and interest lists of items of any trusts proof life insurance and a list of beneficiaries Power of Attorney documentation.
Choosing a NY Medicaid Nursing Home
New York State Medicaid
New York’s Medicaid program provides comprehensive health coverage to more than 7.3 million lower-income New Yorkers Medicaid pays for a wide-range of services, depending on your age, financial circumstances, family situation, or living arrangements. These services are provided through a large network of health care providers that you can access directly using your Medicaid card or through your managed care plan if you are enrolled in managed care. Some services may have small co-payments, which can be waived if you cannot afford them.
Use the link below to see which health insurance options are available to you, including if your income qualifies you for NYS Medicaid.
You May Like: What Airlines Fly To Elmira New York
New Yorks Requirements For Medicaid Qualification
Eligibility for New York Medicaid is something that is determined by a few different factors that have been developed by the New York state department. The benefits given by Medicaid will aid those who are unable to pay their medical bills, such as those on SSI and others who meet the requirements for eligibility. Before those requirements even come in to play though, you first have to fall into one of the following categories:
- Adults who have an income that does not exceed 138% of the FPL
- Infants and/or women who are pregnant whose income does not exceed 218% of the Federal Poverty Level
To qualify for Medicaid – aside from being in one of the preceding two categories – you need to meet predetermined requirements for eligibility. You have to reach, without exceeding certain income thresholds. Additionally, you have to prove that you are a citizen of the US as well as proving that you are a state resident. You also need to have documentation regarding your living situation and your marriage license if you are married, along with your SSN .
Option 3 Download Application
The Department of Health Care Services and Covered California have partnered to create a Single Streamlined Application for affordable health care coverage.
You can use the Single Streamlined Application to apply for a range of affordable health care coverage options, including free or low cost Medi-Cal.
First, , complete it, You can mail your completed and signed application to:
Covered California
Donât Miss: How To Pay A Ticket Online New York
Don’t Miss: Storage Units In Manhattan Ks
What Is Included In A Persons Estate
Under 18 NYCRR 360-7.11, for purposes of Medicaid estate recovery, a persons estate includes anything that they have legal title or interest in at the time of death. This includes real property , personal property , and other assets that are passed to heirs with or without a will. To the extent of a persons interest immediately prior to death, the estate includes assets conveyed to a survivor, heir or assign through a joint tenancy, tenancy in common, survivorship, life estate, living trust or other arrangements. It also includes jointly owned financial institution accounts, jointly held real property, life estate interests, interests in certain trusts and annuities regardless of whether there is a named beneficiary or right of survivorship.
Ny Medicaid Long Term Care Programs
Nursing Home / Institutional Medicaid
Medicaid will cover the cost of long term care in a nursing home for eligible New York residents through its Nursing Home / Institutional Medicaid. This includes payment for room and board, as well as all necessary medical and non-medical goods and services. These can include skilled nursing care, physicians visits, prescription medication, medication management, mental health counseling, social activities and assistance with Activities of Daily Living .
Some of the things that NY Medicaid wont cover in a nursing home are a private room, specialized food, comfort items not considered routine , personal reading items, plants, flowers, and any care services not considered medically necessary.
Any NY Medicaid beneficiary who receives Nursing Home Medicaid coverage must give most of their income to the state to help pay for the cost of the nursing home. They are only allowed to keep a personal needs allowance of $50 / month. This can be spent on any personal item clothes, snacks, books, haircuts, cell phones, etc. It cannot be spent on any item that Medicaid covers, including hygiene basics like toothbrush, soap, deodorant, razors and incontinence supplies, unless the Medicaid beneficiary wants a specific brand that is not covered by Medicaid. In this case, they could spend their personal needs allowance on the item.
Home and Community Based Service Waivers
Disabled, Aged 65+ or Blind / Regular Medicaid
You May Like: Artist Studio For Rent Brooklyn
Eligibility Requirements For New York Medicaid Benefits
In order for New York seniors to be eligible for Medicaid services, they must meet certain financial eligibility requirements. First of all, an individual must be disabled or 65 years of age or older at the time of application.
There are additional requirements for New York Institutional Medicaid. In order for an individual to be eligible to receive New York Institutional Medicaid benefits, he or she must be under the appropriate asset limit set by Medicaid. Those limits are currently as follows:
- Single person $15,150
In the event that only one spouse is seeking admission to a facility, the community spouse will be able to retain at least $74,820or a maximum of one-half of the couples joint liquid assets up to a maximum of $123,600. In the event the assets are over $123,600,there may be other rules that apply.
In Medicaid terminology, the snapshot date refers to the first day of the month on which one spouse goes to a facility, and the assessment of the couples joint liquid assets occurs from this date.
You May Like: How To Get A New York Phone Number
Who Is Eligible For Medicaid In New York
You are categorically eligible for Medicaid if you are:
- A legal U.S. resident. While citizenship is not required, a person must be a legal U.S. resident of the state and county where the application for Medicaid is made to receive benefits. Any applicant not born in the United States must have a physical presence within the state and intend to remain permanently or indefinitely.
- Younger than 21 or older than 65. Any person between the ages of 21 and 65 will only be eligible for Medicaid if they are disabled , certified blind, below the public assistance income and resource levels, or already receiving Supplemental Security Income.
- Below the financial threshold. Medicaid is a “means-tested” benefit program, meaning applicants cannot have enough income or financial resources to pay for their own care.
You May Like: Is There A Casino In New York
Nys Medicaid Related Resources
You may not have heard of these resources available to New Yorkers. Do any of these programs apply to you?
Request a Fair Hearing If you are denied benefits, you have the right to request a fair hearing to explain to a judge why you believe you deserve benefits and your local agency is wrong. The judge may turn you down or may overturn the agencys decision.
Kinship Navigator NYS Kinship Navigator is a referral and advocacy program for family caregivers in New York State. This mainly refers to grandparents, aunts, and uncles who care for a family members children. Kinship Navigator provides legal and medical information and financial assistance when applicable. Visit the website and click on your county for more information.
Eat Smart New York ESNY is a free program for those who receive New York SNAP benefits . The goal is to encourage New Yorkers to eat more fruits and vegetables, drink less sugary beverages, exercise more, and learn to balance caloric intake.
Employment and Training Services The Office of Temporary and Disability Assistance provides employment and training opportunities to those with TA and/or SNAP. Some benefits include child care, transportation, basic education, job skills training, job search and referral assistance, subsidized employment, help paying for work-related expenses , and workplace accommodations if necessary.
for more information about HEAP Heating and Cooling in your county.
How To Apply For Medicaid In Ny
Millions of people all across the United States rely on Medicaid for their health coverage. The program is designed for low-income adults, people with disabilities, and older adults, among others.
Medicaid is sponsored by the government to provide coverage to low-income patients who arenât able to afford medical care otherwise. It is run jointly by both the state and federal governments.
If you live in New York, this article will be an easy to understand guide covering all you need to know about Medicaid in NY.
We will discuss eligibility requirements, what proof you need, the benefits you can receive if eligible, and more.
You May Like: How To Vote Absentee In New York
Eligibility Criteria For Ny Medicaids Long Term Care Programs
To be eligible for NY Medicaid, a person has to meet certain financial requirements and functional requirements. The financial requirements vary by the applicants marital status, if their spouse is also applying for Medicaid and what program they are applying for Nursing Home Medicaid, Home and Community Based Service Waivers or Disabled, Aged 65+ or Blind / Regular Medicaid.
NY Medicaid Nursing Home Medicaid Eligibility Criteria
For married applicants with both spouses applying, the 2022 asset limit for Nursing Home Medicaid through NY Medicaid is $24,600 combined between the two applicants/spouses and the income limit is $1,367 / month combined. For a married applicant with just one spouse applying, the 2022 asset limit is $16,800 for the applicant spouse and $137,400 for the non-applicant spouse, and the income limit is $934 / month for the applicant. The income of the non-applicant spouse is not counted. However, if the income of the non-applicant spouse is greater than $3,435 / month, NY Medicaid will request that 25% of the amount over $3,435 / month be given to the state to help cover the care costs of the applicant spouse. If the non-applicant spouse does not want to do this, they can institute spousal refusal.
NY Medicaid Home and Community Based Services Waivers Eligibility Criteria
NY Medicaid Disabled, Aged 65+ or Blind Medicaid Eligibility Criteria
Information Needed To Apply
To apply, you will need the following information for all applicants, spouse and parents of applying children:
- All household income and employer information including:
Don’t Miss: Does Spirit Fly To New York
Learn About Requirements For Medicaid In New York
To learn how to qualify for Medicaid in New York, applicants need to understand the eligibility requirements set by state and federal guidelines. Obtaining Medicaid benefits eligibility means that applicants have met essential qualifications, such as income level and medical expenses. Unlike Medicare, Medicaid focuses more on income levels instead of age. The program uses federal, state and local funding to provide health insurance to families struggling with purchasing care. The process to qualify for Medicaid involves understanding Medicaid eligibility requirements and knowing what information potential beneficiaries need to provide officials. Once an applicant knows and gathers the necessary details, the process to get benefits starts with an application form. Get answers to the question What are the income requirements for Medicaid in NY? and others by reading the information below.
Who qualifies for Medicaid in New York?
What are the requirements for Medicaid in New York?
To meet qualifications for Medicaid in New York, some applicants will need to demonstrate that their household income falls below a certain percentage of the federal poverty level . However, these specific income levels will depend on the particular Medicaid program for which the applicant qualifies. To learn more about income requirements for Medicaid, .
What are the Medicaid application guidelines in New York?
What are common Medicaid disqualifications in New York?